The
following content is based on the “Accurate Blood Pressure
Measurement” of JNC 7.
Accurate
Blood Pressure Measurement in the Office
The
accurate measurement of BP is the sine qua non for successful
management. The equipment— whether aneroid, mercury, or
electronic—should be regularly inspected and validated. The
operator
should
be trained and regularly retrained in the standardized technique, and
the patient must be properly prepared
and positioned. The auscultatory method
of BP measurement should be used.
- Persons should be seated quietly for at least 5 minutes in a chair (rather than on an exam table), with feet on the floor, and arm supported at heart level. Caffeine, exercise, and smoking should be avoided for at least 30 minutes prior to measurement. Measurement of BP in the standing position is indicated periodically, especially in those at risk for postural hypotension, prior to necessary drug dose or adding a drug, and in those who report symptoms consistent with reduced BP upon standing.
- An appropriately sized cuff (cuff bladder encircling at least 80 percent of the arm) should be used to ensure accuracy. At least two measurements should be made and the average recorded.
- For manual determinations, palpated radial pulse obliteration pressure should be used to estimate Systolic Blood Pressure—the cuff should then be inflated 20–30 mmHg above this level for the auscultatory determinations; the cuff deflation rate for auscultatory readings should be 2 mmHg per second.
- SBP is the point at which the first of two or more Korotkoff sounds is heard (onset of phase 1), and the disappearance of Korotkoff sound (onset of phase 5) is used to define Diastolic Blood Pressure.
- Clinicians should provide to patients, verbally and in writing, their specific BP numbers and the BP goal of their treatment.
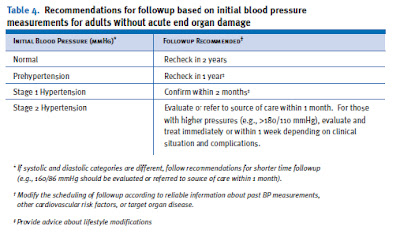
Followup
of patients with various stages of hypertension is
recommended as shown in table 4.
Ambulatory
Blood Pressure Monitoring
Ambulatory
blood pressure monitoring (ABPM) provides information about BP during
daily activities and sleep. BP has a
reproducible “circadian” profile,
with higher values while awake and mentally and physically active,
much lower values during rest and sleep, and early morning increases
for 3 or more hours during the transition of sleep to
wakefulness. These devices use either a microphone
to measure Korotkoff sounds or a cuff that senses arterial waves
using oscillometric techniques. Twenty-four hour BP monitoring
provides multiple readings during all of a patient’s activities.
While office BP values have been used in the numerous studies that
have established the risks associated with an elevated BP and the
benefits of lowering BP, office measurements have some shortcomings.
For example, a white-coat effect (increase in BP primarily in the
medical care environment) is noted in as many as 20–35 percent of
patients diagnosed with hypertension. Ambulatory
BP values are usually lower than clinic readings. Awake hypertensive
individuals have an average BP of >135/85 mmHg, and during sleep,
>120/75 mmHg. The level of BP measurement using ABPM correlates
better than office measurements with
target organ injury ABPM also provides a measure of the percentage of
BP readings that are elevated, the overall BP load, and the extent of
BP fall during sleep. In most people, BP drops by 10–20 percent
during the night; those in whom such reductions are not present
appear to be at increased risk for cardiovascular events. In
addition, it was reported recently that ABPM patients whose 24-hour
BP exceeded 135/85 mmHg were nearly twice as likely to have a
cardiovascular event as those with 24-hour mean BPs <135/85 mmHg,
irrespective of the level of the office
BP.
Indications
for the use of ABPM are listed in table 5. Medicare reimbursement for
ABPM is now provided to assess patients with suspected white-coat
hypertension.
Self-Measurement
Self-monitoring
of BP at home and work is a practical approach to assess differences
between office and out-of-office BP prior to consideration of ABPM.
For those whose out-of-office BPs are consistently <130/80 mmHg
despite an elevated office BP, and who lack evidence of target organ
disease, 24-hour monitoring or drug therapy can be avoided.
Self-measurement
or ABPM may be particularly helpful in assessing BP in smokers.
Smoking raises BP acutely, and the level returns to baseline about 15
minutes after stopping.